Octreotide: patient usage information, precautions and side effects
Tuesday, May 30, 2017 by Gregory Van Dyke
http://www.naturalnewsreference.com/2017-05-30-octreotide-patient-usage-information-precautions-and-side-effects.html
Octreotide: patient usage information, precautions and side effects
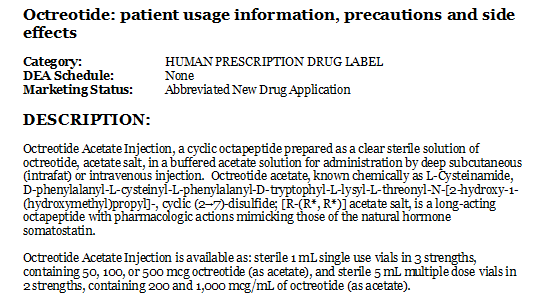
Category: HUMAN PRESCRIPTION DRUG LABEL
DEA Schedule: None
Marketing Status: Abbreviated New Drug Application
DESCRIPTION:
Octreotide Acetate Injection, a cyclic octapeptide prepared as a clear sterile solution of octreotide, acetate salt, in a buffered acetate solution for administration by deep subcutaneous (intrafat) or intravenous injection. Octreotide acetate, known chemically as L-Cysteinamide, D-phenylalanyl-L-cysteinyl-L-phenylalanyl-D-tryptophyl-L-lysyl-L-threonyl-N-[2-hydroxy-1-(hydroxymethyl)propyl]-, cyclic (2→7)-disulfide; [R-(R*, R*)] acetate salt, is a long-acting octapeptide with pharmacologic actions mimicking those of the natural hormone somatostatin.
Octreotide Acetate Injection is available as: sterile 1 mL single use vials in 3 strengths, containing 50, 100, or 500 mcg octreotide (as acetate), and sterile 5 mL multiple dose vials in 2 strengths, containing 200 and 1,000 mcg/mL of octreotide (as acetate).
INDICATIONS AND USAGE:
Acromegaly
Octreotide Acetate Injection is indicated to reduce blood levels of growth hormone and IGF-I (somatomedin C) in acromegaly patients who have had inadequate response to or cannot be treated with surgical resection, pituitary irradiation, and bromocriptine mesylate at maximally tolerated doses. The goal is to achieve normalization of growth hormone and IGF-I (somatomedin C) levels (see DOSAGE AND ADMINISTRATION). In patients with acromegaly, Octreotide Acetate Injection reduces growth hormone to within normal ranges in 50% of patients and reduces IGF-I (somatomedin C) to within normal ranges in 50% to 60% of patients. Since the effects of pituitary irradiation may not become maximal for several years, adjunctive therapy with Octreotide Acetate Injection to reduce blood levels of growth hormone and IGF-I (somatomedin C) offers potential benefit before the effects of irradiation are manifested.
Improvement in clinical signs and symptoms or reduction in tumor size or rate of growth were not shown in clinical trials performed with Octreotide Acetate Injection; these trials were not optimally designed to detect such effects.
Carcinoid Tumors
Octreotide Acetate Injection is indicated for the symptomatic treatment of patients with metastatic carcinoid tumors where it suppresses or inhibits the severe diarrhea and flushing episodes associated with the disease.
Octreotide Acetate Injection studies were not designed to show an effect on the size, rate of growth or development of metastases.
Vasoactive Intestinal Peptide Tumors
(VIPomas)
Octreotide Acetate Injection is indicated for the treatment of the profuse watery diarrhea associated with VIP-secreting tumors. Octreotide Acetate Injection studies were not designed to show an effect on the size, rate of growth or development of metastases.
WARNINGS:
Single doses of octreotide acetate have been shown to inhibit gallbladder contractility and decrease bile secretion in normal volunteers. In clinical trials (primarily patients with acromegaly or psoriasis), the incidence of biliary tract abnormalities was 63% (27% gallstones, 24% sludge without stones, 12% biliary duct dilatation). The incidence of stones or sludge in patients who received octreotide acetate for 12 months or longer was 52%. Less than 2% of patients treated with octreotide acetate for 1 month or less developed gallstones. The incidence of gallstones did not appear related to age, sex or dose. Like patients without gallbladder abnormalities, the majority of patients developing gallbladder abnormalities on ultrasound had gastrointestinal symptoms. The symptoms were not specific for gallbladder disease. A few patients developed acute cholecystitis, ascending cholangitis, biliary obstruction, cholestatic hepatitis, or pancreatitis during octreotide acetate therapy or following its withdrawal. One patient developed ascending cholangitis during octreotide acetate therapy and died.
ADVERSE REACTIONS:
Gallbladder Abnormalities
Gallbladder abnormalities, especially stones and/or biliary sludge, frequently develop in patients on chronic octreotide acetate therapy (see WARNINGS).
Cardiac
In acromegalics, sinus bradycardia (<50 bpm) developed in 25%; conduction abnormalities occurred in 10% and arrhythmias developed in 9% of patients during octreotide acetate therapy (see PRECAUTIONS, GENERAL).
Gastrointestinal
Diarrhea, loose stools, nausea and abdominal discomfort were each seen in 34% to 61% of acromegalic patients in U.S. studies although only 2.6% of the patients discontinued therapy due to these symptoms. These symptoms were seen in 5% to 10% of patients with other disorders.
The frequency of these symptoms was not dose-related, but diarrhea and abdominal discomfort generally resolved more quickly in patients treated with 300 mcg/day than in those treated with 750 mcg/day. Vomiting, flatulence, abnormal stools, abdominal distention, and constipation were each seen in less than 10% of patients.
In rare instances, gastrointestinal side effects may resemble acute intestinal obstruction, with progressive abdominal distension, severe epigastric pain, abdominal tenderness and guarding.
Hypo/Hyperglycemia
Hypoglycemia and hyperglycemia occurred in 3% and 16% of acromegalic patients, respectively, but only in about 1.5% of other patients. Symptoms of hypoglycemia were noted in approximately 2% of patients.
Hypothyroidism
In acromegalics, biochemical hypothyroidism alone occurred in 12% while goiter occurred in 6% during octreotide acetate therapy (see PRECAUTIONS, GENERAL). In patients without acromegaly, hypothyroidism has only been reported in several isolated patients and goiter has not been reported.
Other Adverse Events
Pain on injection was reported in 7.7%, headache in 6% and dizziness in 5%. Pancreatitis was also observed (see WARNINGS and PRECAUTIONS).
Other Adverse Events 1% to 4%
Other events (relationship to drug not established), each observed in 1% to 4% of patients, included fatigue, weakness, pruritus, joint pain, backache, urinary tract infection, cold symptoms, flu symptoms, injection site hematoma, bruise, edema, flushing, blurred vision, pollakiuria, fat malabsorption, hair loss, visual disturbance and depression.
Other Adverse Events < 1%
Events reported in less than 1% of patients and for which relationship to drug is not established are listed: Gastrointestinal: hepatitis, jaundice, increase in liver enzymes, GI bleeding, hemorrhoids, appendicitis, gastric/peptic ulcer, gallbladder polyp; Integumentary: rash, cellulitis, petechiae, urticaria, basal cell carcinoma; Musculoskeletal: arthritis, joint effusion, muscle pain, Raynaud’s phenomenon; Cardiovascular: chest pain, shortness of breath, thrombophlebitis, ischemia, congestive heart failure, hypertension, hypertensive reaction, palpitations, orthostatic BP decrease, tachycardia; CNS: anxiety, libido decrease, syncope, tremor, seizure, vertigo, Bell’s Palsy, paranoia, pituitary apoplexy, increased intraocular pressure, amnesia, hearing loss, neuritis; Respiratory: pneumonia, pulmonary nodule, status asthmaticus; Endocrine: galactorrhea, hypoadrenalism, diabetes insipidus, gynecomastia, amenorrhea, polymenorrhea, oligomenorrhea, vaginitis; Urogenital: nephrolithiasis, hematuria; Hematologic: anemia, iron deficiency, epistaxis; Miscellaneous: otitis, allergic reaction, increased CK, weight loss.
Evaluation of 20 patients treated for at least 6 months has failed to demonstrate titers of antibodies exceeding background levels. However, antibody titers to octreotide acetate were subsequently reported in three patients and resulted in prolonged duration of drug action in two patients. Anaphylactoid reactions, including anaphylactic shock, have been reported in several patients receiving octreotide acetate.
Postmarketing Experience
The following adverse reactions have been identified during the postapproval use of octreotide acetate. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
-
Gastrointestinal: intestinal obstruction
-
Hematologic: thrombocytopenia
DOSAGE AND ADMINISTRATION:
Octreotide Acetate Injection may be administered subcutaneously or intravenously. Subcutaneous injection is the usual route of administration of Octreotide Acetate Injection for control of symptoms. Pain with subcutaneous administration may be reduced by using the smallest volume that will deliver the desired dose. Multiple subcutaneous injections at the same site within short periods of time should be avoided. Sites should be rotated in a systematic manner.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration. Do not use if particulates and/or discoloration are observed. Proper sterile technique should be used in the preparation of parenteral admixtures to minimize the possibility of microbial contamination. Octreotide Acetate Injection is not compatible in Total Parenteral Nutrition (TPN) solutions because of the formation of a glycosyl octreotide conjugate which may decrease the efficacy of the product.
Octreotide Acetate Injection is stable in sterile isotonic saline solutions or sterile solutions of dextrose 5% in water for 24 hours. It may be diluted in volumes of 50 to 200 mL and infused intravenously over 15 to 30 minutes or administered by IV push over 3 minutes. In emergency situations (e.g., carcinoid crisis) it may be given by rapid bolus.
The initial dosage is usually 50 mcg administered twice or three times daily. Upward dose titration is frequently required. Dosage information for patients with specific tumors follows.
Acromegaly
Dosage may be initiated at 50 mcg t.i.d. Beginning with this low dose may permit adaptation to adverse gastrointestinal effects for patients who will require higher doses. IGF-I (somatomedin C) levels every 2 weeks can be used to guide titration. Alternatively, multiple growth hormone levels at 0 to 8 hours after Octreotide Acetate Injection administration permit more rapid titration of dose. The goal is to achieve growth hormone levels less than 5 ng/mL or IGF-I (somatomedin C) levels less than 1.9 U/mL in males and less than 2.2 U/mL in females. The dose most commonly found to be effective is 100 mcg t.i.d., but some patients require up to 500 mcg t.i.d. for maximum effectiveness. Doses greater than 300 mcg/day seldom result in additional biochemical benefit, and if an increase in dose fails to provide additional benefit, the dose should be reduced. IGF-I (somatomedin C) or growth hormone levels should be re-evaluated at 6-month intervals.
Octreotide Acetate Injection should be withdrawn yearly for approximately 4 weeks from patients who have received irradiation to assess disease activity. If growth hormone or IGF-I (somatomedin C) levels increase and signs and symptoms recur, Octreotide Acetate Injection therapy may be resumed.
Carcinoid Tumors
The suggested daily dosage of Octreotide Acetate Injection during the first 2 weeks of therapy ranges from 100 to 600 mcg/day in 2 to 4 divided doses (mean daily dosage is 300 mcg). In the clinical studies, the median daily maintenance dosage was approximately 450 mcg, but clinical and biochemical benefits were obtained in some patients with as little as 50 mcg, while others required doses up to 1,500 mcg/day. However, experience with doses above 750 mcg/day is limited.
VIPomas
Daily dosages of 200 to 300 mcg in 2 to 4 divided doses are recommended during the initial 2 weeks of therapy (range 150 to 750 mcg) to control symptoms of the disease. On an individual basis, dosage may be adjusted to achieve a therapeutic response, but usually doses above 450 mcg/day are not required.
CONTRAINDICATIONS:
Sensitivity to this drug or any of its components.
https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=f278f0d8-4062-420a-97c3-3a8b88253a08
Tagged Under: Tags: chemical medicine, medication, Pharma, Prescription Medicine