Apomorphine: patient usage information, precautions and side effects
Tuesday, May 30, 2017 by Gregory Van Dyke
http://www.naturalnewsreference.com/2017-05-30-apomorphine-patient-usage-information-precautions-and-side-effects.html
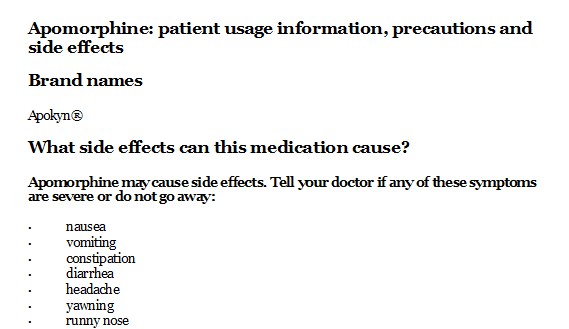
Apomorphine: patient usage information, precautions and side effects
Brand names
Apokyn®
What side effects can this medication cause?
Apomorphine may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
-
nausea
-
vomiting
-
constipation
-
diarrhea
-
headache
-
yawning
-
runny nose
-
weakness
-
paleness
-
flushing
-
bone or joint pain
-
pain or difficulty in urination
-
soreness, redness, pain, bruising, swelling, or itching in the place where you injected apomorphine
Some side effects can be serious. The following symptoms are uncommon, but if you experience any of them, call your doctor immediately:
-
shortness of breath
-
cough
-
fast or pounding heartbeat
-
chest pain
-
swelling of the hands, feet, ankles, or lower legs
-
bruising
-
sudden uncontrollable movements
-
falling down
-
hallucinations (seeing things or hearing voices that do not exist)
-
depression
-
confusion
-
abnormal behavior
-
change in vision
-
painful erection that does not go away
Some laboratory animals who were given apomorphine developed eye disease. It is not known if apomorphine increases the risk of eye disease in humans. Talk to your doctor about the risks of using this medication.
Apomorphine may cause other side effects. Call your doctor if you have any unusual problems while taking this medication.
If you experience a serious side effect, you or your doctor may send a report to the Food and Drug Administration’s (FDA) MedWatch Adverse Event Reporting program online (http://www.fda.gov/Safety/MedWatch) or by phone (1-800-332-1088).
Why is this medication prescribed?
Apomorphine is used to treat ”off” episodes (times of difficulty moving, walking, and speaking that may happen as medication wears off or at random) in patients with Parkinson’s disease (PD; a disorder of the nervous system that causes difficulties with movement, muscle control, and balance) who are taking other medications for their disorder. Apomorphine will not work to prevent ”off” episodes, but will help improve symptoms when an ”off” episode has already begun. Apomorphine is in a class of medications called dopamine agonists. Apomorphine works by mimicking the action of dopamine, a natural substance in the brain that is lacking in patients with PD.
How should this medicine be used?
Apomorphine comes as a solution to inject subcutaneously (just under the skin) and not into a vein. Apomorphine is usually injected when needed, according to your doctor’s directions. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Use apomorphine exactly as directed. Do not use more or less of it or use it more often than prescribed by your doctor.
Your doctor will give you another medication to take when you are using apomorphine. This medication will help decrease your chance of developing upset stomach and vomiting while you are using apomorphine, especially during the beginning of treatment. Your doctor will ask you to begin taking the other medication a few days before you begin to use apomorphine, and to continue taking the other medication for a few months. Do not stop taking the other medication until your doctor tells you to stop.
Your doctor will probably start you on a low dose of apomorphine and gradually increase your dose, not more than once every few days. Ask your doctor what to do if you do not use apomorphine for longer than 1 week. Your doctor will probably tell you to use a low dose and gradually increase your dose again.
Apomorphine solution comes in a glass cartridge to use with an injector pen. Some needles are provided with your pen and additional needles are sold separately. Ask your doctor or pharmacist if you have questions about the type of needle you need. Always use a new, sterile needle for each injection. Never reuse needles and never let a needle touch any surface except the place where you will inject the medicine. Discard used needles in a puncture-resistant container kept out of reach of children. Talk to your doctor or pharmacist about how to discard the puncture-resistant container.
You will receive your first dose of apomorphine in your doctor’s office. After that, you can inject apomorphine yourself or have a friend or relative perform the injections. Your doctor will train the person who will be injecting the medication, and will test him to be sure he can give the injection correctly. Be sure that you and the person who will be giving the injections read the manufacturer’s information for the patient that comes with apomorphine before you use it for the first time at home.
Be sure you know what numbers on the injector pen show your dose. Your doctor may have told you how many milligrams you need to use, but the pen is marked with milliliters. Ask your doctor or pharmacist if you are not sure how to find your dose on the injector pen.
The apomorphine injector pen is only for use by one person. Do not share your pen with anyone.
Be careful not to get apomorphine solution on your skin or in your eyes. If apomorphine does get on your skin or in your eyes, immediately wash your skin or flush your eyes with cold water.
You can inject apomorphine in your stomach area, upper arm, or upper leg. Do not inject into an area where the skin is sore, red, bruised, scarred, infected, or abnormal in any way. Use a different spot for each injection, choosing from among the spots you have been told to use. Keep a record of the date and spot of each injection. Do not use the same spot two times in a row.
To use the apomorphine injector pen, follow these steps:
-
Gather the supplies you will need to give the injection: alcohol swab, injector pen, apomorphine medication cartridge, and new, sterile needle unit. Wash your hands with soap and water.
-
If you already have a medication cartridge in the injector pen, go to step 7 below. To insert a new medication cartridge into the injector pen, follow steps 3-6.
-
Pull off the grey pen cap. Unscrew the cartridge holder from the body of the injector pen.
-
Look at the apomorphine medication cartridge you are going to put into the pen. Check the expiration date to make sure the medication is not expired. Only use a cartridge containing a clear and colorless solution. Do not use a cartridge containing a cloudy or green solution or a solution containing particles. If the apomorphine solution is not clear and colorless, if it contains particles, or if it is expired, do not use it and call your pharmacist.
-
Put the apomorphine cartridge into the cartridge holder. Put in the end with the metal cap first.
-
Lower the body of the pen onto the cartridge holder so that the rod presses against the cartridge plunger. Screw the cartridge holder onto the body of the injector pen. Tighten the pieces until no gap remains and one of the arrows lines up with the marker on the body of the pen.
-
Check the amount of solution in the cartridge through the window in the cartridge holder to be sure there is at least enough solution in the cartridge to give your dose. If the injector pen has been previously used, and the plunger has reached the red line on the cartridge, remove the cartridge and insert a new medication cartridge into the pen, beginning at step 3 above.
-
Remove the paper tab from the back of the needle unit.
-
Hold the injector pen by the cartridge holder and push the needle unit onto the pen. Turn the needle counter-clockwise (to the left) to attach it to the cartridge holder.
-
Remove the outer needle shield with a gentle pull. Save the outer shield. Do not remove the inner needle shield yet. It is still needed to protect the needle.
-
Prime the injector pen to remove air bubbles. To prime, turn the dose knob to 0.1 mL. Carefully remove the inner needle shield and hold the injector pen with the needle pointing up. Hold the needle over a sink or surface that can be wiped easily and firmly push the injection button in as far as it will go and hold for at least 5 seconds. A small stream of medicine should come out of the end of the needle. If a medicine stream does not come out of the needle, repeat this step until a small stream of medicine comes out the end of the needle. Do this step three to four times when you begin to use a new cartridge and once each time you use the cartridge again. If the needle touches anything during the priming process, attach a new sterile needle unit to the injector pen.
-
Set your injection dose by turning the dose knob at the end of the pen until the correct dose (number of mL) is shown in the pen window. The dose will appear as a red number between black lines that line up next to the letters ”mL” on the pen. Make sure the correct number appears in the window. Remember that you are setting your dose in mL (milliliters) and not mg (milligrams). If you are not sure how to set your dose, call your doctor or pharmacist. Never dial the dose or attempt to correct a dialing error while the pen needle is in the skin.
-
If you turn the dose knob past your dose by mistake, do not dial backwards. If you dial backwards, medication will be lost through the needle. To set the correct dose, continue to turn the dial until it is completely turned out. Press the injection button located on the end of the pen. This will reset the dial to zero without pushing medicine out of the needle. Repeat step 12 to set your correct dose.
-
Clean the skin in the area you chose to inject apomorphine with an alcohol swab and allow the skin to air dry.
-
With one hand pinch up about an inch (2.5 centimeters) of skin and fat tissue between your thumb and forefinger at the injection spot. With your other hand, insert the needle all the way into your pinched skin.
-
Push the injection button on the end of the injector pen all the way in. You will hear a clicking sound while the dose is injected. Push the injection button firmly for 5 seconds. Carefully remove the needle from your skin. Be careful not to stick another part of your body when you do this. If medicine is dripping from the needle, do not reinsert the needle. Remember to keep the needle in the skin longer the next time you inject apomorphine. Replace the outer needle shield and go to step 19.
-
If you are unable to push in the injection button, the medication cartridge is empty and no medication is being injected. Remove the needle from your skin, attach the needle shield and discard the needle. Put a new medication cartridge and needle on the injector pen, choose and prepare a new injection site, and complete your injection.
-
If the injection button stops before you receive a complete dose, look at the number in the pen window. Remove the needle from your skin, attach the needle shield and discard the needle. Put a new medication cartridge and needle on the injector pen. Set the injection dose to the number that last appeared in the pen window. Choose and prepare a new injection site, and complete your injection. Try to keep track of the number of times you have used a cartridge so you will know if the cartridge does not contain a complete dose.
-
Place the outer needle shield in the notch on the far left side of your pen carrying case. The opening of the needle shield should be pointing up. Carefully push the injector pen, needle pointing down, into the opening of the outer needle shield.
-
Pick up the pen and hold it by the cartridge holder. Unscrew the pen needle unit from the cartridge holder by turning in a counter-clockwise (to the left) direction. Discard the needle unit properly.
-
Recap the pen. Never recap the pen with a needle attached.
Other uses for this medicine
This medication may be prescribed for other uses; ask your doctor or pharmacist for more information.
What special precautions should I follow?
Before using apomorphine,
-
tell your doctor and pharmacist if you are allergic to apomorphine, sulfa medications, any other medications, or sulfites.
-
do not use apomorphine if you are taking a 5HT3 (serotonin) blocker such as alosetron (Lotronex), dolasetron (Anzemet), granisetron (Kytril), ondansetron (Zofran), or palonosetron (Aloxi).
-
tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking. Be sure to mention any of the following: allergy, cough and cold medications; amiodarone (Cordarone); antidepressants; antihistamines; cisapride (Propulsid); disopyramide (Norpace); diuretics (‘water pills’); dofetilide (Tikosyn); erythromycin (E.E.S., E-Mycin, Erythrocin); haloperidol (Haldol); medications to treat mental illness or upset stomach, heart disease, high blood pressure, pain, or seizures; metoclopramide (Reglan); moxifloxacin (Avelox); muscle relaxants; other medications for Parkinson’s disease; phosphodiesterase inhibitors such as sildenafil (Viagra), tadalafil (Cialis), or vardenafil (Levitra); pimozide (Orap); procainamide (Procanbid, Pronestyl); quinidine (Quinidex); sedatives; sleeping pills; sotalol (Betapace); sparfloxacin (Zagam); tranquilizers; or nitrates such as isosorbide dinitrate (Isordril, Sorbitrate), isosorbide mononitrate (Imdur, ISMO), or nitroglycerin (Nitro-BID, nitro-Dur, Nitroquick, Nitrostat, others). Nitrates come as tablets, sublingual (under the tongue) tablets, sprays, patches, pastes, and ointments. Ask your doctor if you are not sure if any of your medications contain nitrates. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
-
tell your doctor if you drink alcohol or if you have or have ever had asthma; dizziness; eye disease; fainting spells; irregular heartbeat; low blood pressure; mental illness; a sleep disorder; a stroke or mini-stroke, or other brain problems; sudden uncontrolled movements and falls; or heart, kidney, liver, or lung disease.
-
tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while using apomorphine, call your doctor.
-
if you are having surgery, including dental surgery, tell the doctor or dentist that you are using apomorphine.
-
you should know that apomorphine may make you drowsy. Do not drive a car, operate machinery, or do anything that might put you at risk of getting hurt until you know how this medication affects you.
-
you should know that you may suddenly fall asleep during your regular daily activities while you are taking apomorphine. You may not feel drowsy before you fall asleep. If you suddenly fall asleep while you are doing something such as eating, talking, or watching television, call your doctor. Do not drive a car or operate machinery until you talk to your doctor.
-
you should not drink alcohol while you are using apomorphine. Alcohol can make the side effects from apomorphine worse.
-
you should know that apomorphine may cause dizziness, lightheadedness, nausea, sweating, and fainting when you get up too quickly from a lying or sitting position. This is more common when you first start using apomorphine or following an increase in dose. To avoid this problem, get out of bed or get up from a seated position slowly, resting your feet on the floor for a few minutes before standing up.
What special dietary instructions should I follow?
Unless your doctor tells you otherwise, continue your normal diet.
What should I do if I forget a dose?
This medication is usually taken as needed.
What should I know about storage and disposal of this medication?
Keep this medication in the cartridge it came in and out of reach of children. Store the cartridge and injector pen in the carrying case, at room temperature away from dust, moisture (not in the bathroom) and cold or hot temperatures. Never store the pen with a needle attached.
Unneeded medications should be disposed of in special ways to ensure that pets, children, and other people cannot consume them. However, you should not flush this medication down the toilet. Instead, the best way to dispose of your medication is through a medicine take-back program. Talk to your pharmacist or contact your local garbage/recycling department to learn about take-back programs in your community. See the FDA’s Safe Disposal of Medicines website (http://goo.gl/c4Rm4p) for more information if you do not have access to a take-back program.
In case of emergency/overdose
In case of overdose, call your local poison control center at 1-800-222-1222. If the victim has collapsed or is not breathing, call local emergency services at 911.
Symptoms of overdose may include:
-
nausea
-
fainting
-
dizziness
-
blurred vision
-
slow heart beat
-
abnormal behavior
-
hallucinations (seeing things or hearing voices that do not exist)
-
sudden uncontrollable movements
What other information should I know?
Keep all appointments with your doctor.
Do not let anyone else use your medication or injector pen. Ask your pharmacist any questions you have about refilling your prescription.
Apomorphine solution may stain fabric and other surfaces. If you do spill or drip apomorphine solution on a surface, you may wash it with lemon juice to prevent a stain from forming. Bleach will remove apomorphine stains, but should not be used on upholstery.
You may clean your apomorphine pen with a damp cloth as needed. Never use strong disinfectants or wash your pen under running water.
It is important for you to keep a written list of all of the prescription and nonprescription (over-the-counter) medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.
Why is this medication prescribed?
How should this medicine be used?
What special precautions should I follow?
What special dietary instructions should I follow?
What should I do if I forget a dose?
What side effects can this medication cause?
What should I know about storage and disposal of this medication?
Tagged Under: Tags: chemical medicine, medication, Pharma, Prescription Medicine