Cervarix: Human Papillomavirus Bivalent (Types 16 and 18) Vaccine, Recombinant: patient information, prescribing information, ingredients, manufacturer, adverse reactions and side effects
Friday, April 07, 2017 by Gregory Van Dyke
http://www.naturalnewsreference.com/2017-04-07-cervarix-human-papillomavirus-bivalent-types-16-and-18-vaccine-recombinant-patient-information-prescribing-information-ingredients-manufacturer-adverse-reactions-and-side-effects.html
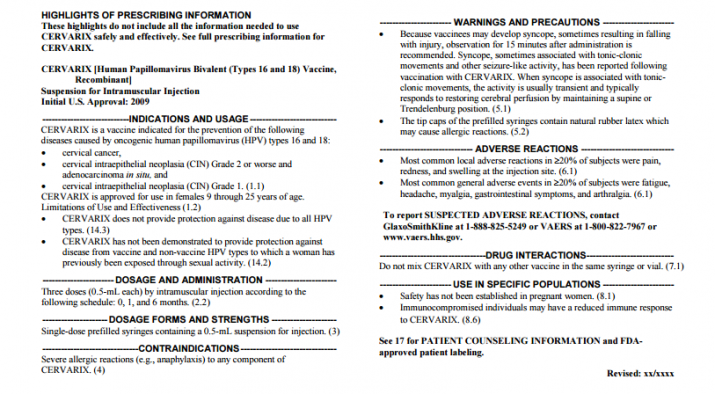
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use CERVARIX safely and effectively. See full prescribing information for CERVARIX.
See full insert sheet at this link at the Natural News Reference website.
CERVARIX [Human Papillomavirus Bivalent (Types 16 and 18) Vaccine, Recombinant]
Suspension for Intramuscular Injection
Initial U.S. Approval: 2009
INGREDIENTS AND EXCIPIENTS
CERVARIX [Human Papillomavirus Bivalent (Types 16 and 18) Vaccine, Recombinant] is a non-infectious recombinant, AS04-adjuvanted vaccine that contains recombinant L1 protein, the major antigenic protein of the capsid, of oncogenic HPV types 16 and 18. The L1 proteins are produced in separate bioreactors using the recombinant Baculovirus expression vector system in a serum-free culture media composed of chemically-defined lipids, vitamins, amino acids, and mineral salts. Following replication of the L1 encoding recombinant Baculovirus in Trichoplusia ni insect cells, the L1 protein accumulates in the cytoplasm of the cells. The L1 proteins are released by cell disruption and purified by a series of chromatographic and filtration methods. Assembly of the L1 proteins into virus-like particles (VLPs) occurs at the end of the purification process. The purified, non-infectious VLPs are then adsorbed on to aluminum (as hydroxide salt). The adjuvant system, AS04, is composed of 3-O-desacyl-4’-monophosphoryl lipid A (MPL) adsorbed on to aluminum (as hydroxide salt).
CERVARIX is prepared by combining the adsorbed VLPs of each HPV type together with the AS04 adjuvant system in sodium chloride, sodium dihydrogen phosphate dihydrate, and Water for Injection.
CERVARIX is a sterile suspension for intramuscular injection. Each 0.5-mL dose is formulated to contain 20 mcg of HPV type 16 L1 protein, 20 mcg of HPV type 18 L1 protein, 50 mcg of the 3-O-desacyl-4’-monophosphoryl lipid A (MPL), and 0.5 mg of aluminum hydroxide. Each dose also contains 4.4 mg of sodium chloride and 0.624 mg of sodium dihydrogen phosphate dihydrate. Each dose may also contain residual amounts of insect cell and viral protein (<40 ng) and bacterial cell protein (<150 ng) from the manufacturing process. CERVARIX does not contain a preservative.
The tip caps contain natural rubber latex; the plungers are not made with natural rubber latex.
INDICATIONS AND USAGE
CERVARIX is a vaccine indicated for the prevention of the following
diseases caused by oncogenic human papillomavirus (HPV) types 16 and 18:
• cervical cancer,
• cervical intraepithelial neoplasia (CIN) Grade 2 or worse and
adenocarcinoma in situ, and
• cervical intraepithelial neoplasia (CIN) Grade 1. (1.1)
CERVARIX is approved for use in females 9 through 25 years of age.
Limitations of Use and Effectiveness (1.2)
• CERVARIX does not provide protection against disease due to all HPV
types. (14.3)
• CERVARIX has not been demonstrated to provide protection against
disease from vaccine and non-vaccine HPV types to which a woman has
previously been exposed through sexual activity. (14.2)
DOSAGE AND ADMINISTRATION
Three doses (0.5-mL each) by intramuscular injection according to the following schedule: 0, 1, and 6 months. (2.2)
DOSAGE FORMS AND STRENGTHS
Single-dose prefilled syringes containing a 0.5-mL suspension for injection. (3)
CONTRAINDICATIONS
Severe allergic reactions (e.g., anaphylaxis) to any component of CERVARIX. (4)
WARNINGS AND PRECAUTIONS
Because vaccinees may develop syncope, sometimes resulting in falling with injury, observation for 15 minutes after administration is recommended. Syncope, sometimes associated with tonic-clonic movements and other seizure-like activity, has been reported following vaccination with CERVARIX. When syncope is associated with tonicclonic movements, the activity is usually transient and typically responds to restoring cerebral perfusion by maintaining a supine or Trendelenburg position. (5.1)
The tip caps of the prefilled syringes contain natural rubber latex which may cause allergic reactions. (5.2)
ADVERSE REACTIONS
Most common local adverse reactions in ≥20% of subjects were pain, redness, and swelling at the injection site. (6.1)
Most common general adverse events in ≥20% of subjects were fatigue, headache, myalgia, gastrointestinal symptoms, and arthralgia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact GlaxoSmithKline at 1-888-825-5249 or VAERS at 1-800-822-7967 or www.vaers.hhs.gov
DRUG INTERACTIONS
Do not mix CERVARIX with any other vaccine in the same syringe or vial. (7.1)
USE IN SPECIFIC LOCATIONS
Pregnancy Category B
Reproduction studies have been performed in rats at a dose approximately 47 times the human dose (on a mg/kg basis) and revealed no evidence of impaired fertility or harm to the fetus due to CERVARIX. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Non-clinical Studies
An evaluation of the effect of CERVARIX on embryo-fetal, pre- and post-natal development was conducted using rats. One group of rats was administered CERVARIX 30 days prior to gestation and during the period of organogenesis (gestation Days 6, 8, 11, and 15). A second group of rats was administered saline at 30 days prior to gestation followed by CERVARIX on Days 6, 8, 11, and 15 of gestation. Two additional groups of rats received either saline or adjuvant following the same dosing regimen. CERVARIX was administered at 0.1 mL/rat/occasion (approximately 47-fold excess relative to the projected human dose on a mg/kg basis) by intramuscular injection. No adverse effects on mating, fertility, pregnancy, parturition, lactation, or embryo-fetal, pre- and post-natal development were observed. There were no vaccine-related fetal malformations or other evidence of teratogenesis.
Clinical Studies
Overall Outcomes: In pre-licensure clinical studies, pregnancy testing was performed prior to each vaccine administration and vaccination was discontinued if a subject had a positive pregnancy test. In all clinical trials, subjects were instructed to take precautions to avoid pregnancy until 2 months after the last vaccination. During pre-licensure clinical development, a total of 7,276 pregnancies were reported among 3,696 females receiving CERVARIX and 3,580 females receiving a control (Hepatitis A Vaccine 360 EL.U., Hepatitis A Vaccine 720 EL.U., or 500 mcg Al(OH)3). The overall proportions of pregnancy outcomes were similar between treatment groups. The majority of women gave birth to normal infants (62.2% and 62.6% of recipients of CERVARIX and control, respectively). Other outcomes included spontaneous abortion (11.0% and 10.8% of recipients of CERVARIX and control, respectively), elective termination (5.8% and 6.1% of recipients of CERVARIX and control, respectively), abnormal infant other than congenital anomaly (2.8% and 3.2% of recipients of CERVARIX and control, respectively), and premature birth (2.0% and 1.7% of recipients of CERVARIX and control, respectively). Other outcomes (congenital anomaly, stillbirth, ectopic pregnancy, and therapeutic abortion) were reported less frequently in 0.1% to 0.8% of pregnancies in both groups.
Outcomes around Time of Vaccination: In pre-licensure studies, sub-analyses were conducted to describe pregnancy outcomes in 761 women (N = 396 for CERVARIX and N = 365 for pooled control, HAV 360 EL.U., HAV 720 EL.U., or 500 mcg Al(OH)3) who received a dose of CERVARIX or control between 45 days prior to and 30 days after the last menstrual period (LMP) and for whom pregnancy outcome was known. The majority of women gave birth to normal infants (65.2% and 69.3% of recipients of CERVARIX and control, respectively). Spontaneous abortion was reported in a total of 11.7% of subjects (13.6% of recipients of CERVARIX and 9.6% of control recipients), and elective termination was reported in a total of 9.7% of subjects (9.9% of recipients of CERVARIX and 9.6% of control recipients). Abnormal infant other than congenital anomaly was reported in a total of 4.9% of subjects (5.1% of recipients of CERVARIX and 4.7% of control recipients), and premature birth was reported in a total of 2.5% of subjects (2.5% of both groups). Other outcomes (congenital anomaly, stillbirth, ectopic pregnancy, and therapeutic abortion) were reported in 0.3% to 1.8% of pregnancies among recipients of CERVARIX and in 0.3% to 1.4% of pregnancies among control recipients.
A post-hoc analysis was performed on a pooled database of pregnancies with known outcome among women 15 to 25 years of age enrolled in controlled clinical trials (N = 4,670 for CERVARIX and N = 4,689 for pooled control, HAV 360 EL.U., HAV 720 EL.U., or 500 mcg Al(OH)3). In an analysis of pregnancies with exposure to CERVARIX or control between 45 days prior to and 30 days after the LMP, the relative risk of spontaneous abortion was 1.54 (95% CI: 0.95, 2.54) for exposure to one dose of CERVARIX (n/N = 46/326) compared with one dose of control (n/N = 33/338) and 1.21 (95% CI: 0.27, 7.33) for exposure to 2 doses of CERVARIX (n/N = 8/71) compared with 2 doses of control (n/N = 3/38).
The association between vaccination with CERVARIX and spontaneous abortion was evaluated in a post-marketing, retrospective, observational, cohort study using primary care medical records in the United Kingdom. The study assessed the risk of spontaneous abortion during weeks 1 to 19 of gestation in two cohorts of women 15 to 25 years of age: one cohort who received one or more doses of CERVARIX between 45 days prior to and 30 days after the LMP (close exposure) and another cohort who received the last dose of CERVARIX between 18 months and 120 days prior to the LMP (remote exposure). The hazard ratio for spontaneous abortion was 1.26 (95% CI: 0.77, 2.09) for the close-exposure cohort (n/N = 23/207) compared with the remote-exposure cohort (n/N = 56/632). In sensitivity analyses for the close-exposure cohort, the hazard ratio compared with the remote-exposure cohort was 1.07 (95% CI: 0.61, 1.86) for women who received only one dose of CERVARIX (n/N = 17/178) and 2.59 (95% CI: 1.11, 6.04) for women who received 2 doses of CERVARIX (n/N = 6/29).
Nursing Mothers
In non-clinical studies in rats, serological data suggest a transfer of anti–HPV-16 and anti–HPV- 18 antibodies via milk during lactation in rats. Excretion of vaccine-induced antibodies in human milk has not been studied for CERVARIX. Because many drugs are excreted in human milk, caution should be exercised when CERVARIX is administered to a nursing woman.
Pediatric Use
Safety and effectiveness in pediatric patients younger than 9 years of age have not been established. The safety and effectiveness of CERVARIX have been evaluated in 1,275 subjects 9 through 14 years of age and 6,362 subjects 15 through 17 years of age. [See Adverse Reactions (6.1), Clinical Studies (14.5).]
Geriatric Use
Clinical studies of CERVARIX did not include sufficient numbers of subjects 65 years of age and older to determine whether they respond differently from younger subjects. CERVARIX is not approved for use in subjects 65 years of age and older.
Immunocompromised Individuals
The immune response to CERVARIX may be diminished in immunocompromised individuals [see Drug Interactions (7.3)].
Safety has not been established in pregnant women. (8.1)
Immunocompromised individuals may have a reduced immune response to CERVARIX. (8.6)
Revised: xx/xxxx
https://www.fda.gov/downloads/BiologicsBloodVaccines/Vaccines/ApprovedProducts/UCM186981.pdf
Tagged Under: Tags: Cervarix, dosage, ingredients, insert sheet, side effects, usage, warnings